For those unaware, one of the most hotly contested issues in sex therapy is whether or not sex addiction is a useful diagnosis and whether it even actually exists as a distinct addictive process in the first place. This controversy receives lots of coverage in the media and I am often contacted by journalists for expert opinions (check out this recent article in Prevention Magazine, for example, it’s pretty good).
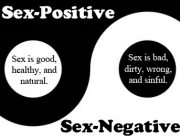
I don’t think that anyone argues that sexual behavior can be problematic or feel “out of control.” Indeed, the Out of Control Sexual Behavior (OCSB) model is gaining a lot of traction in therapist circles. The main concern with the sex addiction model, however, is that by placing sexuality alongside toxic and dangerous substances such as alcohol and hard drugs, it unduly stigmatizes sexual expression as inherently dangerous, taking us back to the Victorian dark ages of sexual repression. For this reason, one of the common criticisms of the sex addiction field is that clinicians untrained in human sexuality diagnose and pathologize individuals who stray from heteronormative and mononormative sexual expressions as struggling with mental pathology. Of course, there must be a middle ground between unquestioning validation and trigger-happy pathologization. Earlier this summer, the World Health Organization (WHO) sought to find this median by releasing their latest International Classification of Diseases (ICD) 11.
There’s a lot that’s positive in the new ICD 11 classification, and also consistent with the American Association of Sex Educators, Counselors, and Therapist’s (AASECT) ‘s position statement on sex addiction (and I should know, I was one of four co-authors of the position statement). Let’s go through it in more thorough detail (you can reach the synopsis here).
First, WHO uses the terminology “compulsive” rather than “addiction” and classifies it as an impulse control disorder. This is significant because sex addiction proponents for years have tried unsuccessfully to point to some kind of biological basis for sex addiction, similar to substance dependence. The WHO classification makes it clear that this is not the case. The terms addiction and compulsion are often conflated, but the difference is important since addictionologists often advocate for an abstinence-only approach to treatment to get the “brain chemicals balanced” or some other pseudoscientific explanation. To this point, there has been no evidence of a chemically dependent sexual response akin to substance dependence. Proponents of the addiction model will argue that dopamine and endorphins are released during pleasure, but these same chemicals are released during pleasurable things such as eating cake or watching a beautiful sunset. It is unclear how the process is radically different in terms of the neurochemicals involved in sex and riding roller coasters.
Second, WHO makes explicit that the diagnosis is not related to moral judgments and disapproval. This is significant because a large segment of individuals who show up for sex addiction treatment are individuals who are morally upset with their fetishes or use of porn, or their partner is. Indeed, paraphilias (fetishes) have been specifically excluded from the criteria. Recent research shows that those who have moral difficulty with their sexual behavior (mostly, but not exclusively for religious reasons, for example) are more likely to identify as sex addicts, irrespective of the frequency of the problematic sexual behavior.
In addition, the ICD description eliminates people who identify as sex addicts simply because they were caught cheating or having an affair because they would have needed to persistently fail in controlling their impulses. Many folks who have made bad decisions may be drawn to a mental health diagnosis such as sex addiction as a means of taking away personal responsibility from destructive behaviors such as infidelity. Rather than seeing oneself as the victimizer, sex addiction provides these individuals with a useful label of victimhood. Instead of taking personal responsibility, they can now find fault in their childhood and any other myriad of historical difficulties, even if they are historically accurate and true. I certainly don’t want to insinuate that a history of childhood abuse could not influence individuals to misbehave, but I am providing a reason why the sex addiction diagnosis has gained social currency and popularity that goes well beyond grounded science.
Indeed, much of the criticism of the sex addiction model is that it employs junk science to lump a bunch of disparate behaviors (foot fetishists, adulterers, and people uncomfortable with porn) all under one label while prescribing a one-size fits all approach to treatment. The experience of many former sex addiction patients I have worked with is that everyone who goes into a sex addiction clinic gets a diagnosis. The ICD classification makes it clear we are dealing with compulsivity, not a biological addiction, and adds specific criteria to exclude individuals who should not be diagnosed, which is most of them.
Which then leads to the question of how should we approach working with individuals who have wreaked havoc on their lives and the lives of others due to their sexual behaviors? I have written much on this topic, which you can access here and here and here, but fundamentally I want to start with a mindset of exploration and curiosity rather than all-knowing labeling. Sexuality is very complex and the same behaviors could have radically different meanings for the individuals involved. You can have ten people engaged in the same sexual behavior, but for ten drastically different reasons. So, it is important to stay open-minded and curious and proceed from a sexologically informed perspective. Often those struggling with out of control sexual behavior qualify for a dual diagnosis, meaning they are primarily struggling with another mental health issue such as depression, anxiety, or OCD, and the sexual behavior is a symptom, not the disease.
If we get too stuck on the labeling and judging the behavior, we may miss the big picture, and leave the individual actually feeling more shamed and compulsive than when he or she first came in. Tons of research suggests that compulsivity is highly linked to shame. Think about it, if I told you to never think of a pink elephant because that would be terrible, are you more or less likely to find yourself thinking of the pink elephant? You need to think of it just to think about what you are trying to avoid! And the more you resist, the more you become hyperfocused and obsessed about it, leading to an intensifying obsessive-compulsive cycle. Rather, good sex therapy involves placing the sexual behavior within an accurate contextual and systemic framework and understanding its deeper, underlying meaning to the individual. Once we rush to place labels, we’ve already shut down the conversation. For this reason, sex addiction is often a case of too much certainty clouding the mental health field’s pursuit of knowledge.















































































 Prevention: Is Sex Addiction Real?
Prevention: Is Sex Addiction Real? Romper: Emotional Infidelity
Romper: Emotional Infidelity Fatherly: BDSM More Common Than You Think
Fatherly: BDSM More Common Than You Think E! Online: Marrying a Murderer
E! Online: Marrying a Murderer Who Magazine: What is Bisexuality?
Who Magazine: What is Bisexuality? CNN: Why Men May Exaggerate Their Sex Numbers
CNN: Why Men May Exaggerate Their Sex Numbers Women’s Health: 10 Kinky Sex Ideas
Women’s Health: 10 Kinky Sex Ideas NY Post: How Tattoos Can Sabotage Your Love Life
NY Post: How Tattoos Can Sabotage Your Love Life Allure: 8 BDSM Sex Tips to Try If You’re a Total Beginner
Allure: 8 BDSM Sex Tips to Try If You’re a Total Beginner
 Great article in Prevention Magazine about the sex addiction controversy. Check out what I had to say.
Great article in Prevention Magazine about the sex addiction controversy. Check out what I had to say.
 Romper approached me again for another quote, this time about emotional infidelity.
Romper approached me again for another quote, this time about emotional infidelity.
 Interesting piece in Fatherly about BDSM in which I was interviewed.
https://www.fatherly.com/love-money/bdsm-kinky-sex-not-uncommon/
Interesting piece in Fatherly about BDSM in which I was interviewed.
https://www.fatherly.com/love-money/bdsm-kinky-sex-not-uncommon/ E! News picked up my an interview I did with Vice a few years ago about hybristophilia, which is the attraction to criminals. Very interesting story.
E! News picked up my an interview I did with Vice a few years ago about hybristophilia, which is the attraction to criminals. Very interesting story.
 Who is Australia's version of People Magazine. They wanted to know what bisexuality is and I provided some insight.
Who is Australia's version of People Magazine. They wanted to know what bisexuality is and I provided some insight.
 Seems like something doesn't add up on sex surveys-- are men exaggerating their number of partners? Check out what I tell CNN.
Seems like something doesn't add up on sex surveys-- are men exaggerating their number of partners? Check out what I tell CNN.
 Women's Health asked me for some kinky ideas to spice up one's sex life.
Women's Health asked me for some kinky ideas to spice up one's sex life.
 I was interviewed by the NY Post about all the ways in which I've seen bad tattoos sabotage relationships.
I was interviewed by the NY Post about all the ways in which I've seen bad tattoos sabotage relationships.
 Allure Magazine asked me about tips for BDSM beginners.
Allure Magazine asked me about tips for BDSM beginners.
 I answer questions from Salon.com about the infamous porn site PornHub.
I answer questions from Salon.com about the infamous porn site PornHub.
 I tell Cosmo about the personality traits of monogamous individuals.
I tell Cosmo about the personality traits of monogamous individuals.
 I explain to Refinery29 why it's so important to not fake orgasms in a relationship.
I explain to Refinery29 why it's so important to not fake orgasms in a relationship.
 I am interviewed in this fairly nuanced piece on the pros and cons of porn.
I am interviewed in this fairly nuanced piece on the pros and cons of porn.
 I am interviewed by Headspace, one of the best meditation and mindfulness apps available, on how to become more present.
https://www.headspace.com/blog/2017/05/26/enjoy-sex-more/
I am interviewed by Headspace, one of the best meditation and mindfulness apps available, on how to become more present.
https://www.headspace.com/blog/2017/05/26/enjoy-sex-more/ I am interviewed in this intriguing Business Insider article on how often happy couples have sex.
I am interviewed in this intriguing Business Insider article on how often happy couples have sex.
 The Huffington Post in South Africa profiles my work around challenging sex addiction (including my red/yellow/green menu exercise) .
The Huffington Post in South Africa profiles my work around challenging sex addiction (including my red/yellow/green menu exercise) .
 I go deep into the sex toy business with Vice.
I go deep into the sex toy business with Vice.
 I give some insight into this interesting topic.
https://thetab.com/us/2017/03/22/happens-boyfriend-leaves-another-man-63306
I give some insight into this interesting topic.
https://thetab.com/us/2017/03/22/happens-boyfriend-leaves-another-man-63306 I am featured in this outstanding article in UK's Independent on women and virtual reality porn. I thought this was a fairly sharp and nuanced piece.
I am featured in this outstanding article in UK's Independent on women and virtual reality porn. I thought this was a fairly sharp and nuanced piece.
 I give Redbook some pointers on having a 3some for the first time.
I give Redbook some pointers on having a 3some for the first time.
 Playboy sent a journalist to watch Fifty Shades Darker, and then compared the movie with the results from my recent groundbreaking research on BDSM. Great article, enjoy!
Playboy sent a journalist to watch Fifty Shades Darker, and then compared the movie with the results from my recent groundbreaking research on BDSM. Great article, enjoy!
 I am featured in this terrific New York Magazine article, discussing some of the finer points brought up in the earlier article in SELF magazine (see listing below).
I am featured in this terrific New York Magazine article, discussing some of the finer points brought up in the earlier article in SELF magazine (see listing below).
 I am featured in this terrific article in SELF magazine on the nuances of the sex addiction debate.
I am featured in this terrific article in SELF magazine on the nuances of the sex addiction debate.
 Complex asked me to weigh in on this provocative topic.
Complex asked me to weigh in on this provocative topic.

 I weigh in in this great advice column in Thrillist by Elle Stanger.
I weigh in in this great advice column in Thrillist by Elle Stanger.

 Great episode, check it out.
https://soundcloud.com/futureofsex/04-exploring-sexual-fluidity-bicuriousity-for-women-featuring-skirt-club-and-dr-michael-aaron
Great episode, check it out.
https://soundcloud.com/futureofsex/04-exploring-sexual-fluidity-bicuriousity-for-women-featuring-skirt-club-and-dr-michael-aaron I give couples advice on how to deal with differences in preferred sleeping arrangements.
I give couples advice on how to deal with differences in preferred sleeping arrangements.
 Alternet does a great job of reviewing my book. Check out the link below.
Alternet does a great job of reviewing my book. Check out the link below.
 In this episode, we talk about the societal myths of sexuality, including:
In this episode, we talk about the societal myths of sexuality, including:
 I was asked to appear on Australian radio. It was a very fun segment, will post the link when I have it!
I was asked to appear on Australian radio. It was a very fun segment, will post the link when I have it! I appear on the Stereo-Typed podcast to discuss my new book, fantasies, and our shadow self. Click the audio player below and enjoy!
https://www.spreaker.com/user/crazyheart/stereo-typed-8-dancing-with-your-shadow
I appear on the Stereo-Typed podcast to discuss my new book, fantasies, and our shadow self. Click the audio player below and enjoy!
https://www.spreaker.com/user/crazyheart/stereo-typed-8-dancing-with-your-shadow I appear on the Boom Doctors Podcast to discuss my new book Modern Sexuality and my work as a sex therapist. Clink the link below to listen in.
http://theboomdoctors.com/2016/09/21/ep-132-michael-aaron-on-his-work-as-a-sex-therapist-his-new-book-modern-sexuality/
I appear on the Boom Doctors Podcast to discuss my new book Modern Sexuality and my work as a sex therapist. Clink the link below to listen in.
http://theboomdoctors.com/2016/09/21/ep-132-michael-aaron-on-his-work-as-a-sex-therapist-his-new-book-modern-sexuality/ I was asked by Nylon Magazine to weigh in on the subject of porn and what it means about the individual consumer. Pretty good non-pathologizing piece, check it out here:
I was asked by Nylon Magazine to weigh in on the subject of porn and what it means about the individual consumer. Pretty good non-pathologizing piece, check it out here:
 I was interviewed by Vocativ about a new virtual reality series entitled "Virtual Sexology," designed to provide breathing and relaxation exercises in a virtual reality format to help individuals improve sexual functioning. Will something like this prove effective? The jury is out, but check out what I had to say...
I was interviewed by Vocativ about a new virtual reality series entitled "Virtual Sexology," designed to provide breathing and relaxation exercises in a virtual reality format to help individuals improve sexual functioning. Will something like this prove effective? The jury is out, but check out what I had to say...
 I appeared on the nationally broadcasted Fusion Network Hotline show to discuss the GOP platform of porn as a "public health crisis." As part of the discussion I debate Dr. Neil Malamuth on porn and sexual violence. I thought this was a very thorough and productive half hour, which you can watch below:
I appeared on the nationally broadcasted Fusion Network Hotline show to discuss the GOP platform of porn as a "public health crisis." As part of the discussion I debate Dr. Neil Malamuth on porn and sexual violence. I thought this was a very thorough and productive half hour, which you can watch below:
 In this Huffington Post article, I advise couples to use sex menus to spice things up. Check out all the details in the link below.
In this Huffington Post article, I advise couples to use sex menus to spice things up. Check out all the details in the link below.

 I appeared on French national tv channel Canal + on the Emission Antoine tv show, discussing the psychology behind financial domination. I will post a video clip of the interview shortly.
I appeared on French national tv channel Canal + on the Emission Antoine tv show, discussing the psychology behind financial domination. I will post a video clip of the interview shortly. I was interviewed on Huffington Post's Love + Sex Podcast, which I'm told is the most downloaded sex and relationship podcast on iTunes. In this episode, I dispel the wild myths about "sex roulette" parties.
I was interviewed on Huffington Post's Love + Sex Podcast, which I'm told is the most downloaded sex and relationship podcast on iTunes. In this episode, I dispel the wild myths about "sex roulette" parties.
 I was interviewed for an upcoming online sexuality discussion series, the Sexual Reawakening Summit. It features many top sex therapists from around the country and you can access it by using this link:
I was interviewed for an upcoming online sexuality discussion series, the Sexual Reawakening Summit. It features many top sex therapists from around the country and you can access it by using this link:  In the April edition of my Men's Fitness 'Sex Files' Q&A column, I answer questions about anal sex and porn. Hurry and pick up a copy before it's off the stands!
In the April edition of my Men's Fitness 'Sex Files' Q&A column, I answer questions about anal sex and porn. Hurry and pick up a copy before it's off the stands!

 I was asked by Women's Health Magazine to provide some advise on how to incorporate some new positions to spice up one's sex life. With a bunch of pictures and diagrams, I'm sure you'll find something that will intrigue you.
I was asked by Women's Health Magazine to provide some advise on how to incorporate some new positions to spice up one's sex life. With a bunch of pictures and diagrams, I'm sure you'll find something that will intrigue you.
 Looks like Yahoo News picked up the Reuters article on women's fears that their partners expect sexual perfectionism. Check it out.
Looks like Yahoo News picked up the Reuters article on women's fears that their partners expect sexual perfectionism. Check it out.
 My latest interview with Reuters, this time about social pressure on women to be perfect sexually. "Our society is filled with sexual myths and misconceptions, mostly stemming from a combination of our culture's puritanical roots, as well as rampant consumerism, which feeds off individual insecurities to sell unnecessary products," Aaron said.
My latest interview with Reuters, this time about social pressure on women to be perfect sexually. "Our society is filled with sexual myths and misconceptions, mostly stemming from a combination of our culture's puritanical roots, as well as rampant consumerism, which feeds off individual insecurities to sell unnecessary products," Aaron said.
 Head out to the newsstands and grab a copy of the Jan 2016 issue of Men's Fitness Magazine to see the premier of the new monthly "Sex Files" column in which I answer readers' sex questions. In this month's issue I answer a question in which a guy is looking to help his girlfriend enjoy more pleasure when she is having sex on top. Check out the screenshot below to see my response:
Head out to the newsstands and grab a copy of the Jan 2016 issue of Men's Fitness Magazine to see the premier of the new monthly "Sex Files" column in which I answer readers' sex questions. In this month's issue I answer a question in which a guy is looking to help his girlfriend enjoy more pleasure when she is having sex on top. Check out the screenshot below to see my response:

 Love& is a new magazine about relationships and sex. They interviewed me about common things that women may want their guys to improve upon in the bedroom. One of the big ones is touch, as a lot of men are way too rough and don't know how to adjust their touch to what their partner wants. For more on this, and other pointers, check out the article itself below:
Love& is a new magazine about relationships and sex. They interviewed me about common things that women may want their guys to improve upon in the bedroom. One of the big ones is touch, as a lot of men are way too rough and don't know how to adjust their touch to what their partner wants. For more on this, and other pointers, check out the article itself below:
 Market analysts predict that new virtual reality technology will revolutionize the way we experience media, and will specifically boost the porn industry to unprecedented levels. This detailed article covers a lot of ground, addressing both the technology, business and social ramifications of virtual reality porn. I was asked to give my take on the issue and somehow a 20 minute phone conversation was distilled to a brief paragraph at the end of the piece, but nonetheless, it is still a worthwhile read.
Market analysts predict that new virtual reality technology will revolutionize the way we experience media, and will specifically boost the porn industry to unprecedented levels. This detailed article covers a lot of ground, addressing both the technology, business and social ramifications of virtual reality porn. I was asked to give my take on the issue and somehow a 20 minute phone conversation was distilled to a brief paragraph at the end of the piece, but nonetheless, it is still a worthwhile read.
 Does Bill Cosby have a fetish for unconscious women? Who knows? He's not a client and I've never met him, so I cannot say for sure, but this provocative piece in the NY Times tries to get to the bottom of his alleged bizarre behavior. The reporter did a great job dealing with some uncomfortable material, so be sure to click the link below to see what I had to say on this issue:
Does Bill Cosby have a fetish for unconscious women? Who knows? He's not a client and I've never met him, so I cannot say for sure, but this provocative piece in the NY Times tries to get to the bottom of his alleged bizarre behavior. The reporter did a great job dealing with some uncomfortable material, so be sure to click the link below to see what I had to say on this issue:
 I was recently asked by a reporter from Men's Fitness magazine to discuss reasons why a heterosexual man might refrain from having sex with a willing woman. The questions were basically soft balls, seemingly aimed at a younger, more inexperienced, male audience, but hey, I managed to drop a few decent pointers, relating to finding out if the woman is in a relationship, and if so, what kind of relationship she is in before diving in. If you want to take a look and poke around more, you can go directly to the article below. You are going to have to click to page 3 to see my quotes, btw.
I was recently asked by a reporter from Men's Fitness magazine to discuss reasons why a heterosexual man might refrain from having sex with a willing woman. The questions were basically soft balls, seemingly aimed at a younger, more inexperienced, male audience, but hey, I managed to drop a few decent pointers, relating to finding out if the woman is in a relationship, and if so, what kind of relationship she is in before diving in. If you want to take a look and poke around more, you can go directly to the article below. You are going to have to click to page 3 to see my quotes, btw.
 I was recently interviewed for a Men's Health article on sex toys designed for men. They wanted to know my take on these "robotic masturbators" (as they called them) and as always, I tried to take a fair and balanced view of things. I pointed out that they could be used as a way to get better acquainted with one's sexuality (as well as get some much needed relief), but an over-reliance on technology may also limit guys from developing the necessary skills that would help them form romantic relationships.
At any rate, hurry on over to the article here--
I was recently interviewed for a Men's Health article on sex toys designed for men. They wanted to know my take on these "robotic masturbators" (as they called them) and as always, I tried to take a fair and balanced view of things. I pointed out that they could be used as a way to get better acquainted with one's sexuality (as well as get some much needed relief), but an over-reliance on technology may also limit guys from developing the necessary skills that would help them form romantic relationships.
At any rate, hurry on over to the article here--  Go check out a great, and I mean GREAT, absolutely fascinating article in the May issue of Upscale Magazine, entitled "Secret Lovers," in which I am interviewed regarding the hush hush world of the swinger subculture. The writer does a really good job of trying to understand the psychology of folks who practice consensual non-monogamy and I think the piece is very even-handed, with some practical tips for couples who are curious about dipping their toes in the lifestyle. I'll leave you with a quote from one of the swingers profiled in the piece, which I think gives a good feel for the tone and depth of the article-- "I love to see her with two guys and two girls at once. I enjoy submissive women, and there is no sexier submission than to watch my wife please me by pleasing others." If that sounds interesting, then I suggest you head out and grab a copy. It's well worth the read.
Go check out a great, and I mean GREAT, absolutely fascinating article in the May issue of Upscale Magazine, entitled "Secret Lovers," in which I am interviewed regarding the hush hush world of the swinger subculture. The writer does a really good job of trying to understand the psychology of folks who practice consensual non-monogamy and I think the piece is very even-handed, with some practical tips for couples who are curious about dipping their toes in the lifestyle. I'll leave you with a quote from one of the swingers profiled in the piece, which I think gives a good feel for the tone and depth of the article-- "I love to see her with two guys and two girls at once. I enjoy submissive women, and there is no sexier submission than to watch my wife please me by pleasing others." If that sounds interesting, then I suggest you head out and grab a copy. It's well worth the read. I am featured in the Sex Q&A section of Cosmo's April 2014 issue, in which I get asked about BJs, Plan B, sex in hot tubs, and all kinds of other tittilating reader questions. They did a good job of adding all kinds of humor, including a silly picture of tea bags-- need I say more? It's a can't- miss hoot. Go and check it out at news stands now!
I am featured in the Sex Q&A section of Cosmo's April 2014 issue, in which I get asked about BJs, Plan B, sex in hot tubs, and all kinds of other tittilating reader questions. They did a good job of adding all kinds of humor, including a silly picture of tea bags-- need I say more? It's a can't- miss hoot. Go and check it out at news stands now! I just recently did an interview for a cool podcast called
I just recently did an interview for a cool podcast called